The Mental Health Paradox: An Exploration
The term mental health paradox describes the peculiar reality where, despite heightened awareness and resources surrounding mental health, many individuals still fail to access the help they need, or they experience stigma that prevents them from fully engaging in support systems. This paradox paints a complex picture of societal progress and its shortcomings in addressing one of humanity’s most pressing concerns.
The Rising Awareness vs. the Growing Crisis
In many ways, society has made significant strides in understanding mental health. Campaigns and initiatives have brought once-taboo topics into public discourse. Social media platforms, blogs, and mental health apps have become tools of awareness and education. However, while mental health resources appear more accessible than ever, the paradox emerges: the demand for mental health services often outpaces the availability and quality of care (World Health Organization [WHO], 2021).
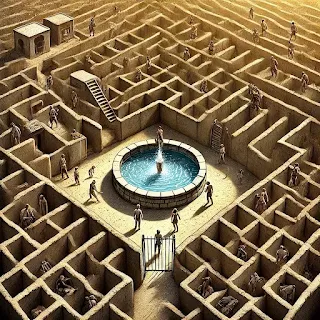
It’s like filling a reservoir intended to serve a growing population. The water represents mental health resources, and though more is added, it cannot keep up with the swelling needs of those seeking support. Awareness has grown, but stigma continues to loom large, creating invisible walls that many are unable or unwilling to cross (National Alliance on Mental Illness [NAMI], 2022). Furthermore, resources are still scarce. In rural areas especially, the lack of mental health professionals leaves people stranded without adequate support, like watching a lifeboat sail just out of reach while they remain stuck on a deserted island.
Economic barriers exacerbate the issue. Therapy and mental health services are costly, and even those with insurance often face high deductibles and copays, leaving many to feel as though the care they need is an unattainable luxury (WHO, 2021).
Populations Most Affected by the Mental Health Paradox
Marginalized Communities: The Invisible Struggle
Marginalized populations—including people of color, LGBTQ+ individuals, and those from low-income backgrounds—face disproportionate barriers to mental health care. Systemic inequities compound their struggles, creating layers of complexity that often go unaddressed (The Journal of Psychiatric Services, 2021).
For instance, African Americans and Hispanic individuals are less likely to receive mental health services than their white counterparts, even when experiencing similar levels of distress. Language barriers, cultural stigma, and mistrust in healthcare systems make the path to support feel like a maze where some paths are blocked or hidden (The Journal of Psychiatric Services, 2021).
Youth and Adolescents: The Future in Crisis
Teenagers and young adults are particularly vulnerable to the paradox. The pressures of academic achievement, social media comparison, and societal expectations have created a mental health crisis among this age group. Suicide remains the second-leading cause of death for individuals aged 10-24 in the United States (NAMI, 2022). Despite targeted awareness campaigns, many adolescents struggle silently, unable to articulate their feelings or fearing they won’t be taken seriously. Social media amplifies these struggles by exposing young minds to a constant stream of idealized lives that make their own feel inadequate.
Rural Populations: The Distant Help
In rural areas, geographic isolation often leads to limited access to mental health care. Telehealth offers potential, but it isn’t a perfect solution. Many rural residents lack reliable internet connections, leaving them feeling isolated from care. This situation creates a sense of abandonment, as though help is within sight but just beyond their grasp (WHO, 2021).
Factors Behind the Mental Health Paradox
Stigma: The Unseen Weight
Stigma continues to act as a formidable barrier to mental health care. While public conversations around mental health have grown louder, societal expectations that dismiss struggles—like "just tough it out" or "others have it worse"—weigh people down. This persistent judgment feels like an anchor tied to a swimmer’s ankle, dragging them deeper into their struggles and further from recovery (NAMI, 2022).
Economic Disparities: The Cost of Care
The cost of mental health services often puts them out of reach for those in need. Therapy sessions can cost hundreds of dollars, and even with insurance, the financial burden remains significant. This financial barrier leaves many people to feel as though the mental health care they desperately need exists only in a world they cannot afford to access (WHO, 2021).
Cultural Norms and Misunderstandings
In many cultures, mental health is either not acknowledged or seen as a personal failing. This deeply ingrained resistance discourages individuals from recognizing the need for help or supporting others in their mental health journeys (The Journal of Psychiatric Services, 2021).
Strategies to Address the Paradox
Reducing Stigma Through Education
Schools, workplaces, and community organizations must prioritize mental health education to break down misconceptions. Sharing personal stories and supporting peer advocacy can make seeking help feel less daunting (NAMI, 2022).Improving Accessibility
Governments and private sectors must invest in telehealth infrastructure, affordable care options, and mental health training for professionals in underserved areas (WHO, 2021).Targeted Support for Vulnerable Populations
Tailored programs for marginalized groups, including cultural competency training for providers, can help bridge the gap in care (The Journal of Psychiatric Services, 2021).Encouraging Preventative Care
Just as annual physicals are routine, mental health check-ins should become a normalized part of healthcare. Early intervention can prevent crises before they arise (NAMI, 2022).
A Shared Responsibility
The mental health paradox highlights both the strides we’ve made and the gaps we still need to bridge. Addressing this issue requires a collective effort—from individuals prioritizing their mental health to governments investing in equitable healthcare systems. Only by acknowledging the complexities of the paradox can we work toward a world where mental health care is not a privilege but a universal right.
References
National Alliance on Mental Illness. (2022). Mental health by the numbers. Retrieved from https://www.nami.org
The Journal of Psychiatric Services. (2021). Disparities in mental health service use.
World Health Organization. (2021). Mental health: Strengthening our response. Retrieved from https://www.who.int


Comments
Post a Comment